Good news for the three people in New York City who last week tested negative for the coronavirus; however, the global health crisis is escalating. The situation is fluid and currently, according to the Centers for Disease Control (CDC), Arizona, California, Illinois, Massachusetts, Washington and Wisconsin are the U.S. states that have reported confirmed cases of the disease. A CDC-developed laboratory test kit to detect 2019 novel coronavirus (2019-nCoV) began shipping last week to select qualified U.S. and international laboratories.
At press time Reuters reported that “the number of new coronavirus deaths on the Chinese mainland rose to 1,011 by the morning of Feb. 11, surpassing that of the SARS epidemic in 2002/2003. On Feb. 10, the new deaths reached another daily record at 108, pushing the total well over the 774 who died from SARS, or Severe Acute Respiratory Syndrome. Of the recent coronavirus deaths, 103 were in China’s central Hubei province, where the virus has infected most people. New deaths in Hubei’s capital Wuhan, where the outbreak started, saw a rare decline,” said Reuters. The number infected is greater than 40,000.
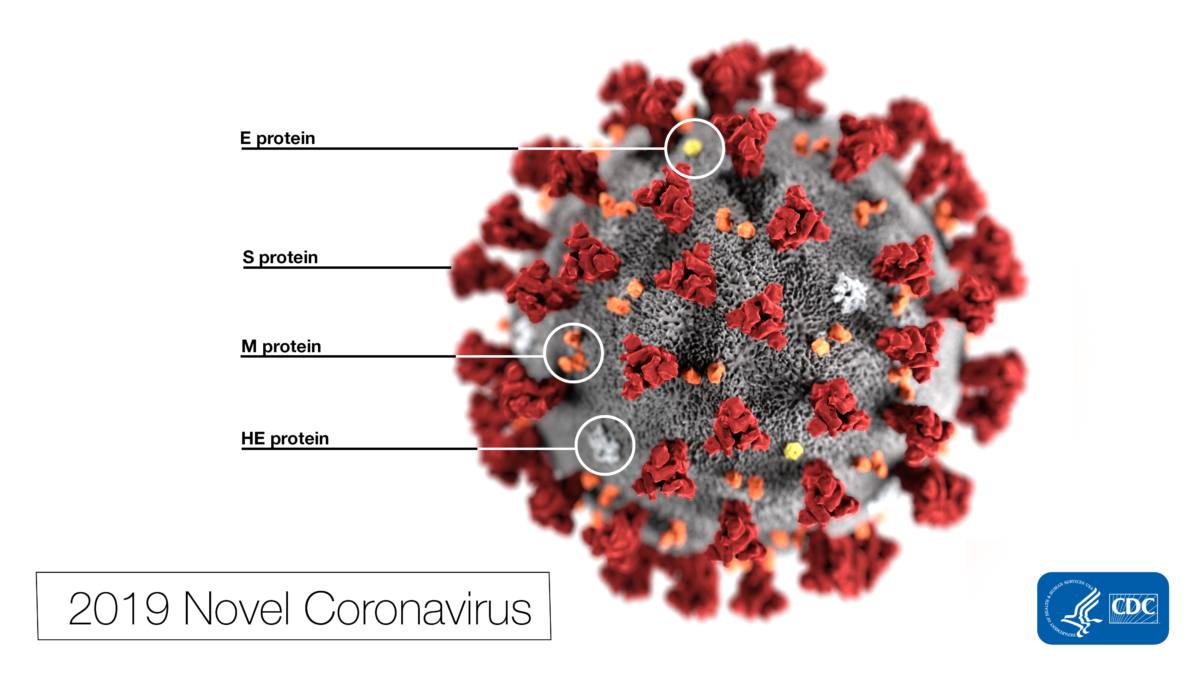
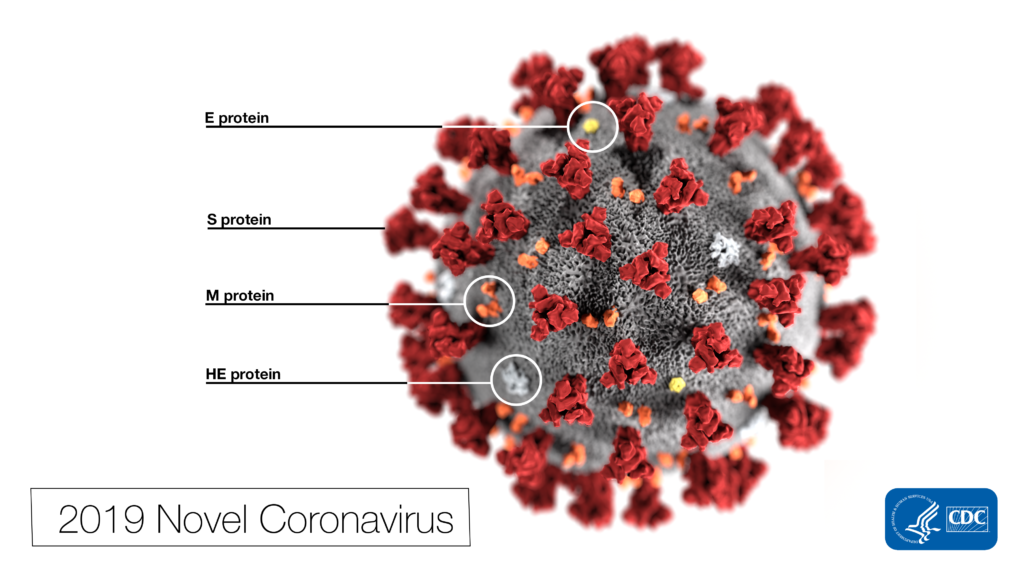
Coronaviruses are a large family of viruses ranging from the common cold to much more serious diseases and can infect both humans and animals. What precautions should the teams overseeing U.S. healthcare facilities and medical office buildings be taking to protect employees, patients and their families?
The CDC notes human coronaviruses are most commonly spread from an infected person to others through the air by coughing and sneezing; close personal contact, such as touching or shaking hands; touching an object or surface with the virus on it, then touching your mouth, nose or eyes before washing your hands; and rarely, fecal contamination.
There are currently no vaccines to protect against human coronavirus infections, but the CDC has developed two checklists that identify key actions that can be taken now to enhance preparedness for potential or confirmed patients with 2019 novel coronavirus.
The CDC also suggests helping to reduce risk of infection by taking the following familiar precautions:
• Wash your hands often with soap and water for at least 20 seconds.
• Avoid touching your eyes, nose, or mouth with unwashed hands.
• Avoid close contact with people who are sick.
• Stay home while you are sick.
U.S. healthcare organizations can mitigate the risk of an outbreak of the coronavirus by preparing now and being ready even if there is little empirical evidence to suggest a case will arrive at their facility. That’s the advice offered by the Healthcare Financial Management Association (HFMA).
For example, HFMA urges all hospitals to be taking precautions ASAP to screen and isolate patients who present with a fever or upper respiratory symptoms and who have been to China recently or have been in contact with anyone who has.
“If a facility does not have the resources or capabilities, it’s time for the organization’s leadership to reach out to a neighboring facility, the state’s public health department or CDC,” according to the HFMA. Chuck Alsdurf, HFMA’s director of healthcare finance policy, operational initiatives, notes that many organizations are ready and willing to collaborate to ensure there’s a defined plan if a case does occur in their state. Often there are monies held aside for these types of risks and it’s a relatively easy process to manage in terms of funding or reimbursement after the fact. Even with some other funding sources available, there’s still a cost to preparing, though it’s rarely less expensive to be unprepared.
