Candida auris is an emerging fungus that presents a serious global health threat, according to the CDC website. Healthcare facilities in several countries have reported that C. auris has caused severe illness in hospitalized patients. Some strains of Candida auris are resistant to all three major classes of antifungal drugs. This type of multidrug resistance has not been seen before in other species of Candida. Also of concern, C. auris can persist on surfaces in healthcare environments and spread between patients in healthcare facilities, unlike most other Candida species. CDC has developed Interim Recommendations to help prevent the spread of C. auris.
The CDC website reports: “C. auris is difficult to identify with standard laboratory methods and can be misidentified in labs without specific technology. CDC encourages all U.S. laboratory staff who identify C. auris strains to notify their state or local public health authorities and CDC at candidaauris@cdc.gov. Find answers to frequently asked questions about C. auris on our questions and answers page and in the Candida auris: Interim Recommendations.
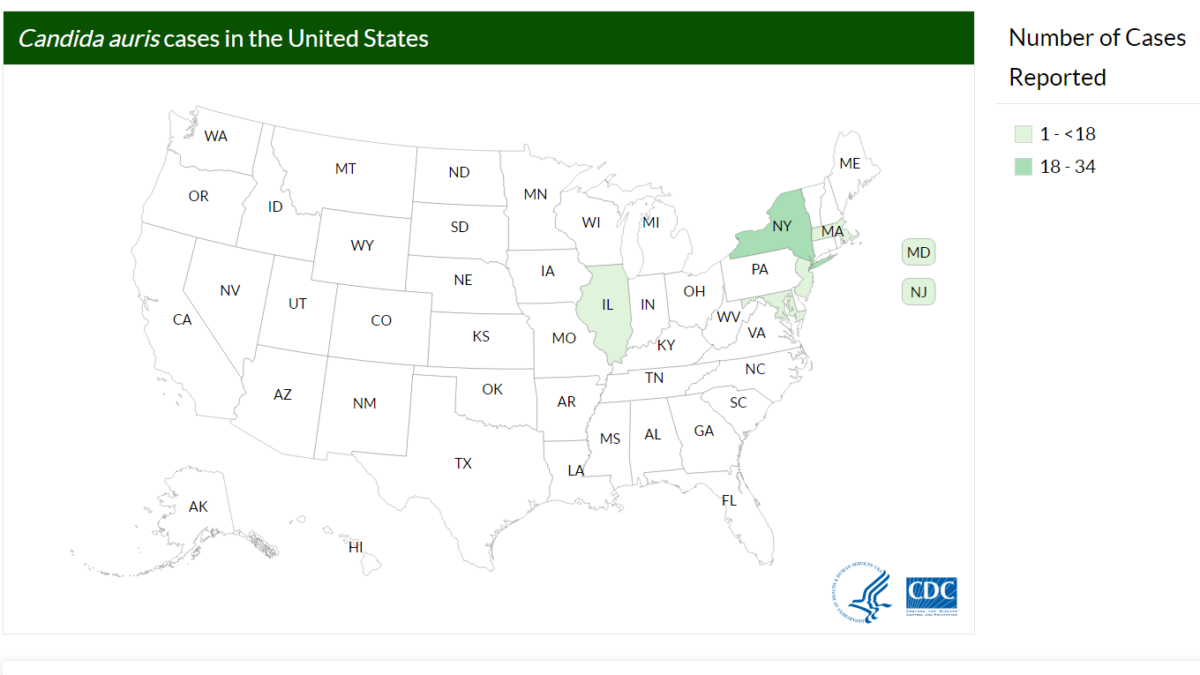
CDC is working with state and local health departments to identify and investigate cases of C. auris. The following map displays where C. auris cases have been identified in the United States as of March 16, 2017. This map will be updated monthly.”
Reporting
Healthcare facilities that suspect they have a patient with C. auris infection should contact state or local public health authorities and CDC (candidaauris@cdc.gov).
Infection Control Measures
What infection control measures should be used for patients with C. auris infection and for patients colonized with C. auris?
In acute-care settings, such as acute-care hospitals, providers should place patients with C. auris infection or colonization in single rooms on Standard and Contact Precautions[PDF – 226 pages].
In general, residents in nursing homes who are colonized or infected with C. auris should be housed in single rooms when available and placed on Contact Precautions. Residents do not need to be restricted to their rooms, but they should perform hand hygiene before exiting their rooms. If residents colonized or infected with C. auris use shared equipment (e.g., physical therapy equipment, recreational resources), items that residents handle extensively should be cleaned and disinfected after use.
Highly functional nursing home residents without wounds or indwelling medical devices (e.g., urinary and intravenous catheters and gastrostomy tubes) who can perform hand hygiene might be at lower risk of transmitting C. auris. Facilities may consider relaxing the requirement for Contact Precautions for these residents. However, in these instances, healthcare personnel should still use gowns and gloves when performing tasks that put them at higher risk of contaminating their hands or clothing. These tasks include changing wound dressings and linens and assisting with bathing, toileting, and dressing in the morning and evening.
When patients are transferred to other healthcare facilities, receiving facilities should receive notification of C. auris infection or colonization and the level of precautions recommended.
In addition, state or local health authorities and CDC should be consulted about the need for additional interventions to prevent transmission.
How long should infected or colonized patients remain on infection control precautions?
The optimal duration for use of infection control precautions in healthcare settings (acute-care hospitals, long-term acute-care hospitals, and nursing homes) is unclear since the typical duration of C. auris colonization is unknown. Periodic reassessments for presence of C. auris colonization (e.g., every 1–3 months) might be needed to inform duration of infection control measures. Assessments of colonization should involve testing of axilla and groin swabs for C. auris. Two or more assessments performed at least one week apart with negative results are needed before discontinuing infection control precautions is considered; the patient or resident should not be on antifungal medications active against C. auris at the time of these assessments. Note that decisions to discharge the patient from one level of care to another should be based on clinical criteria and the ability of the accepting facility to provide care and not on the presence or absence of colonization.
How should rooms of patients with C. auris be cleaned?
C. auris can persist on surfaces in healthcare environments. Healthcare facilities that have patients with C. auris infection or colonization should ensure thorough daily and terminal cleaning and disinfection of these patients’ rooms. CDC recommends use of an Environmental Protection Agency (EPA)-registered hospital-grade disinfectant effective against Clostridium difficile spores (List K). This is a change from the original recommended for use of a disinfectant with a fungal claim. CDC’s interim disinfection recommendation for C. auris will continue to be updated as new information becomes available.”

